Cognitive Behavioural Therapy (CBT) is considered ‘the current gold standard in the psychotherapy field.’ Since its development in the 1960s, CBT has become increasingly popular in the treatment of a range of different types of emotional distress. This form of therapy is particularly effective as it can be applied inside and outside the treatment room.
Alongside formal engagements with a set course of CBT, it is possible to supplement cognitive behavioural therapy with self-taught techniques using manuals readily available to the general public. This allows individuals to feel more empowered about their treatment and can also work to eliminate potential access barriers.
Call our admissions line 24 hours a day to get help.
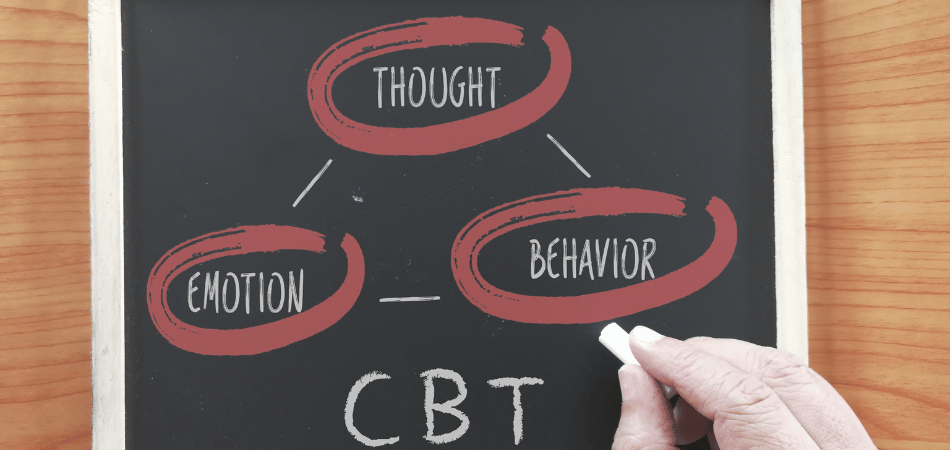
What is cognitive behavioural therapy?
Cognitive Behavioural Therapy is a branch of psychotherapy, a ‘method for the treatment of mental disorders and psychological problems.’
- Cognitive refers to thinking.
- Behavioural refers to doing.
This kind of therapy, then, aims to help us assess and combat how our thoughts and feelings may be negatively impacting us.
The key tenet of CBT is the idea that our thoughts and feelings are heavily linked to our behaviours and vice versa. CBT teaches that our internal experiences do not exist in a vacuum. Our feelings and behaviours are often driven by thoughts – impulsive or otherwise. These can, in turn, be impacted by beliefs, values or ideas about ourselves, our history, and how we view the world.
The aim of all of this is to establish greater awareness and, therefore, a stronger sense of control. This can help to reduce the prevalence of a range of pervasive symptoms, including:
- Maladaptive behaviours (things that can be harmful, such as binge drinking, using drugs or self-harm)
- Absolute or ‘black and white thinking’
- Unhealthy thought cycles
- Disproportionate emotional responses
What is CBT used for?
CBT is a widely used therapeutic intervention for a range of mental health conditions, such as:
- Anxiety
- Bipolar disorder
- Depression
- Obsessive-compulsive disorder (OCD)
- Phobias
- Post-traumatic stress disorder (PTSD)
- Post and perinatal mental health problems
- Psychosis
- Schizoaffective disorder
- Schizophrenia
CBT is utilised in cases of treatment-resistant conditions. For example, if you have engaged in talking therapy to combat depression in the past and have found that the same issues recur over time, then CBT can be a useful intervention. This is because CBT has been aligned with shifting deep-set thought patterns and extreme emotional responses.
The versatility of CBT also makes it useful for individuals dealing with a dual diagnosis. If you are in treatment for more than one condition, you are clinically considered to have a dual diagnosis, which can be defined as ‘the temporal co-existence of two or more psychiatric disorders.’
A large number of individuals dealing with substance abuse disorders have an additional diagnosis or one or more mental health conditions. An estimated 70% of individuals dealing with drug addiction experience problems with their mental health. For those addicted to alcohol, the number rises to 86%. Common dual diagnoses in these contexts include depression, anxiety, bipolar disorder, borderline personality disorder and schizophrenia.
CBT can also be used to help individuals dealing with difficulties in specific areas of their lives, including:
- chronic stress
- eating disorders
- hoarding
- self-harm
- issues with sleep
As addiction can sometimes coexist with these behaviours, Cognitive Behavioural Therapy can help alleviate engagement with these harmful behaviours through the reevaluating of similarly maladaptive thoughts.
Call our admissions line 24 hours a day to get help.
Cognitive Behavioural Therapy: In theory
A series of key theories underpin Cognitive Behavioural Therapy. These elements build the foundation for CBT in clinical practice.
Cognitive distortions
One of the main areas that CBT combats is ‘cognitive distortions.’ Cognitive distortions are beliefs that are ‘beliefs that are negatively biassed, inaccurate and rigid.’ The thoughts that grow from cognitive distortion can be implicitly or explicitly harmful. By recognising when a cognitive distortion is at play, we can begin to challenge difficult thoughts. The aim is that this challenge can shorten the circuit of previously harmful patterns of thought – and subsequent behaviours in reaction to these.
There are a series of cognitive distortions that you encounter in CBT. These can include:
- black and white thinking (things are one thing or another, difficulty appreciating nuance)
- blaming (always registering the blame for an outcome in yourself)
- catastrophising (focusing on the worst outcome)
- discounting the positive (minimising the importance of the positive)
- emotional reasoning (reacting based on feelings rather than thought)
- mind reading (believing we know what other people are thinking)
- overgeneralisation (using situations we have encountered to make general, rigid rules)
- predictive thinking (working with hypotheticals; attempting to predict outcomes)
- ‘should’ and ‘must’ statements (applying rigid rules to a situation, thought or feeling)
The role of cognitive distortions was identified by Aaron Beck, the psychiatrist who developed CBT.
Automatic thoughts
CBT teaches us that the problem with difficult thought patterns is that they generally happen unconsciously. When we have been thinking in a particular way for so long, it is hard to break these patterns of thought. That is why CBT puts so much focus on the idea of learning about different kinds of thoughts in order to begin to challenge them. Like with anything else, it can take practice. However, persistence is worthwhile; recognising which cognitive distortions tend to colour your thinking can be a valuable tool in recovery.
CBT hopes to teach patients to recognise when thoughts are ‘exaggerated, distorted, mistaken or unrealistic.’ Often, we can go for a long time without realising that our thoughts are ‘dysfunctional.’ By addressing this, we can start to work on challenging these negative thoughts and, therefore, loosen their hold upon us.
Beliefs
The third key area in CBT lies in the realm of beliefs. When we think about something often enough, we can begin to believe it. This belief then colours subsequent thoughts and approaches to situations throughout our lives. CBT suggests that there are two key types of beliefs: core beliefs and intermediate beliefs.
Core beliefs are our ‘central ideas about the self and the world.’ These are the beliefs that perhaps colour out thinking the most often.
Intermediate beliefs are shorter-term beliefs that often show a core belief in action.
For example, your core belief may be that you are ‘not good enough.’ An intermediate belief as a result of that could be that you ‘need to work harder than everyone else’ in order to achieve acceptance. Analysis like this can help to identify dysfunctional core beliefs. By beginning to investigate these further, you can increase your chances of toppling them.
Cognitive Behavioural Therapy: in practice
CBT is typically conducted in hour-long appointments. These are available in 1-1 contexts or as group sessions. In some instances, CBT practices can be incorporated into specific types of family therapy.
CBT may feel different to other therapies, to begin with. This is because it has a series of set practices that can help you approach specific life occurrences. That means that CBT sessions may feel slightly less ‘free-flowing’ to begin with. Your therapist may emphasise the role of structure and focus attention on specific recurring ideas or issues. For example, if your therapist notes that you consistently return to feelings of guilt, then you may find that they begin to hone in on the topic of guilt as an overarching theme of concern in your life.
The structure of CBT can work differently depending on your needs and the style of your therapist. However, it typically works around a loose chronology:
- Identifying key issues
- Unpicking the key thoughts, beliefs and behaviours to challenge
- Finding healthier and safer thoughts, beliefs and behaviours
- Applying these thoughts, beliefs and behaviours in relevant situations
- Continually allowing yourself to notice or ‘take stock’ of your feelings
Alongside learning about the key cognitive distortions and beliefs that colour your thinking, you may also be introduced to specific mindful practices. This is especially common in a specific thread of CBT, known as Mindfulness-Based Cognitive Therapy (MCBT). This type of CBT can help you to stay more present and practice noticing your thoughts and feelings before reacting to them.
Cognitive Behavioural Therapy for Addiction
There are a number of Cognitive Behavioural Therapy benefits that naturally apply in the context of addiction. CBT can be particularly helpful in controlling impulses and strong emotions. Both of these are very prominent in cases of addiction.
Studies have shown that CBT is particularly effective in treating alcohol addiction, as well as addictions to cocaine, opioids and cannabis. It has also been used in some instances of polydrug use. CBT has been shown to be most helpful in addiction treatment when it focuses on ‘target[ing] maladaptive behavioural patterns, motivational and cognitive barriers to change, and skill deficits.’ In these cases, the CBT ‘tool kit’ can be described as a particular apt method of care for individuals dealing with addiction.
CBT can be difficult to engage with, given the level of self-reflection required to facilitate the therapy effectively. For that reason, it may be beneficial to access CBT following a detox period. Following detox, individuals often feel more in control, more ‘balanced’ and have a greater sense of calm in comparison to before. Once cravings have been quelled for the short term, we can then turn to CBT to establish ways to resist cravings moving forward. This combination approach to addiction has been shown to have the greatest treatment outcomes, suggesting the power of engaging with multiple types of therapy during time in rehab.
How effective is CBT?
We are all unique individuals with our own unique sets of needs, beliefs, preferences and idiosyncrasies. This means that whilst CBT may be life-changing for one patient, others may find that it is not the appropriate form of support for them. The Royal College of Psychiatrists estimates that 1 in 4 patients drop out of CBT before finishing the full course of treatment. There are conversations around the effectiveness of CBT that suggest patients who are able to articulate their feelings with greater clarity are more likely to benefit from this type of support than others.
For this reason, CBT could be helpful following the use of other forms of talking therapy, such as counselling, when individuals have better practice at sharing, identifying and sharing their feelings. However, the statistic from The Royal College identifies that 75% of those entering CBT engage with the full course of treatment. That suggests a high attainment rate in this particular type of therapy.
Some people may find that they need to return to CBT – this does not mean that they have failed, but rather that a ‘top-up course’ of support could provide a refresher of the skills that have previously been learnt.
Call our admissions line 24 hours a day to get help.
CBT: The benefits
CBT has been associated with improvements in a variety of areas relating to psychological well-being, including:
- developing self esteem and improved confidence
- decreasing base levels of anxiety and depression
- minimising instances of crisis
- reducing engagement with maladaptive behaviours
- allowing individuals to feel more in control
- inspiring people to feel hopeful about their future
These shifts can help people to create a genuine change in their lives. Whether this is visible as a reduction in panic attacks, an improvement in mood or a reduced need to turn to substances, the benefits of CBT can manifest in very powerful ways.
Accessing CBT
If you or someone in your life is struggling with their mental health – or perhaps with an addiction – you may benefit from engaging with CBT. CBT is a mode of inclusive support that puts the client’s needs at the centre. Specialist clinicians operate under the understanding that each and every person deserves to feel happy, healthy, safe and in control. The goal of therapy is to help people achieve that control in the times when they may need it most.
CBT is a key foundation of mental health and addiction treatments offered across the globe. You can access CBT as an inpatient or outpatient care to suit your current circumstances. Cognitive Behavioural Therapy could be the first big step in your move towards recovery, clarity, and a greater sense of control.
Call our admissions line 24 hours a day to get help.